Healthremedy123.com – There is a wide variety of criteria for evaluating finger joint involvement in Rheumatoid Arthritis. Most commonly, doctors refer to the FOIAS to grade the severity of this disease. The FOIA is a semiquantitative grading scale based on individual joint scores from 0 to 3. The criteria were applied to 30 joints in each patient: the bilateral wrist, metacarpophalangeal joints I-V, and the proximal and distal interphalangeal joints II-V. The combined scores for both hands were calculated and analyzed by two investigators.
Using High-Resolution US for Finger Joint Imaging
US scans of the finger joints are used in both early and advanced RA patients. Compared to clinical examinations, high-resolution US scans are more sensitive and can be performed at less cost than MRI. Ideally, both techniques should be used, but there is some disagreement as to which is more accurate. In most cases, it’s best to use the high-resolution US for finger joint imaging.
FOIs can measure inflammation in the finger joints and wrists. FOI is a sensitive, non-invasive method of monitoring therapy. The FOI is highly sensitive and reflects inflammation at an early stage of the disease. If a positive FOI is found, it means the disease is subclinical. However, a study by Werner et al. found that this method could detect early inflammation in 45% of clinically asymptomatic joints.
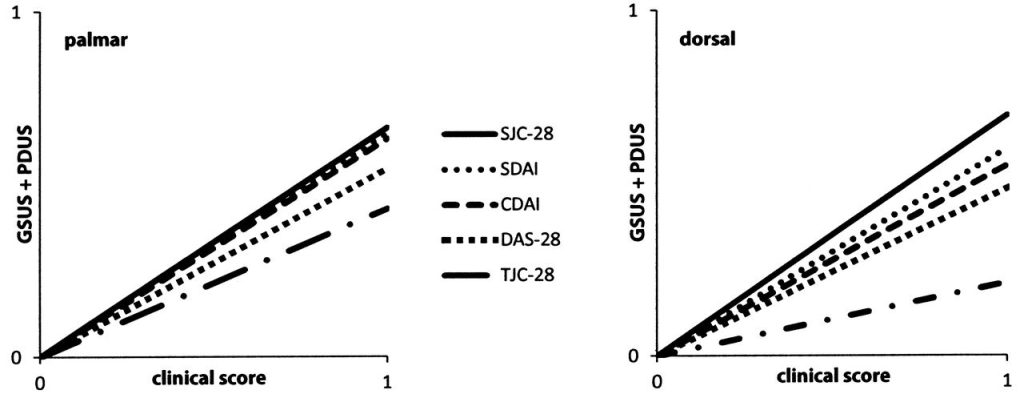
In the present study, PDUS findings in the dorsal aspect of finger joints were more common than in the palmar side. In both types of Rheumatoid Arthritis, tenosynovitis and hypervascularization were observed. In both of these methods, GSUS and PDUS findings of synovitis were interpreted semi-quantitatively. GSUS grading defined an anechoic line beneath the joint capsule. PDUS grading defined a presence of two or more single color signs in the synovial region. Both MCP II and PD III had a similar incidence of erosions.

However, conventional imaging methods are not able to reliably assess the early stages of the disease. While conventional imaging methods provide a valid assessment of synovitis, they are insufficient in sensitivity to detect the disease in its early stages. Contrast-enhanced magnetic resonance imaging (CE-MRI) provides detailed information about inflammation in the joints and predicts disease progression at an early stage. However, the CE-MR method is expensive and time-consuming for routine screening. Optic molecular imaging is a promising alternative to contrast MRI for early RA detection. Unlike CT or MRI, optical molecular imaging uses no ionizing radiation and is non-invasive.
A Promising Alternative to MRI Contrast Early Detection of RA
Although the frequency distribution of the inflammatory changes in the joints in both OA and RA patients was similar, there were differences between the two groups. PDUS and FOI revealed the presence of greater inflammatory changes in the RA patients. Moreover, both OA and RA patients had similar frequencies for grade two and three in the inflammatory scores of the respective joints. As these findings show, both conditions are associated with a high degree of joint damage, and they can be used as an aid in diagnosis.
The goal of treatment for RA is to minimize joint damage and improve the quality of life of RA patients. The main objective is to prevent loss of function, minimize disability, and reduce cardiovascular events. RA prevalence varies from country to country, but overall, it is less common in rural areas. In the Rochester study, 71.5% of women and 50% of men had positive findings for the rheumatoid factor and anticitrullinated protein. The SDAI composite scores were 26.6, 27.4, and 26 respectively.
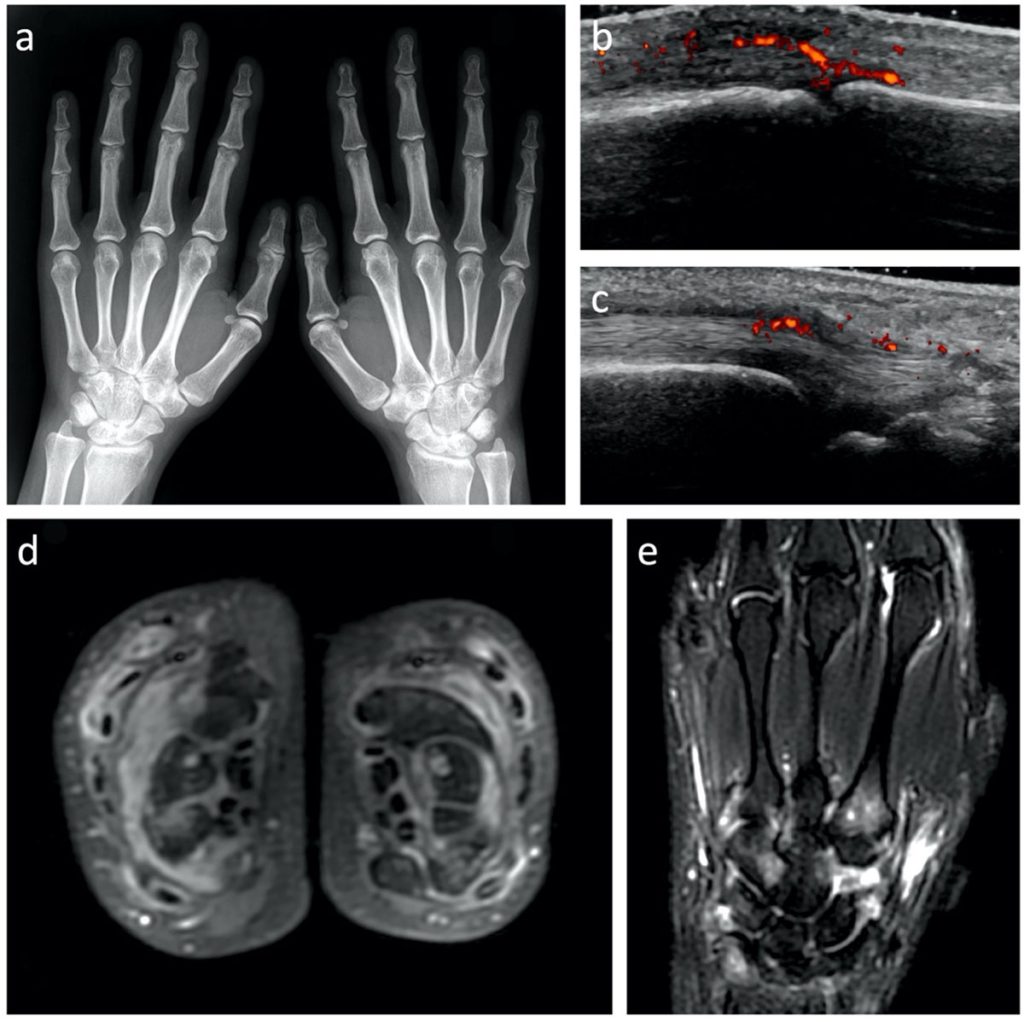
The US7 synovitis score was the best predictor of erosions, although it was not able to differentiate articular cartilage from bone. The DAS28 has also proved to be a poor predictor of erosions. Besides, the US7 score was correlated with the ESR during 12 months of follow-up. The GSUS was a more reliable method for assessing the damage in hand joints than the US5 score.
Dorsal GSUS Detects More Double Positive Synovitis and Joints
The dorsal GSUS detected significantly more synovitis and double-positive joints than the palmar GSUS. The dorsal GSUS, on the other hand, detected positive findings in 44.7% of joints. At six months, the dorsal GSUS showed more than half of patients with the disease. At six months, the numbers had decreased by 66% and to 11.2% in the dorsal GSUS.
Radiographic imaging has become the gold standard in the assessment of the progression of RA disease. Major radiographic indicators of joint damage include joint space narrowing, periarticular osteoporosis, and bony erosions. The US7 score includes Larsen and Sharp scores and alterations. Moreover, the Sharp score focuses on the extent of joint erosions and joint space narrowing.
Reference:


