Healthremedy123.com – The Posterior Fossa is a part of the brain that supports the cerebellum. Approximately 20% of all pediatric cancers are brain tumors. Of these, the most common are medulloblastoma, cerebellar astrocytoma, and ependymoma. Recent advances in molecular genetics have allowed a new proposed classification. According to this classification, the tumors affect the brainstem, the cerebellum, and the cranial vault. This knowledge is important for determining the most appropriate treatment for each child.
How to Predict the Risk of Neurocognitive Disorders
In addition to predicting whether or not a patient will develop neurocognitive impairment, serial MRI scan of the posterior fossa can help predict the risk of neurocognitive impairment. Researchers in the Japanese journal Asian Pac J Cancer Prev reported the results of a study of patients with recurrent tumors of the posterior fossa. They used multiple discriminant analysis and MRI to identify the most likely patient subtype.
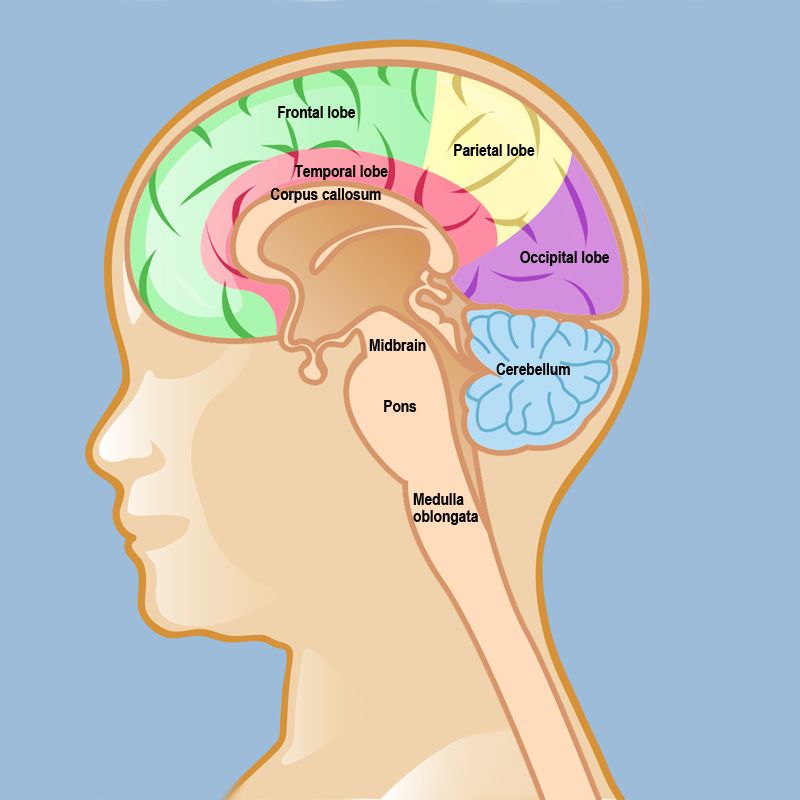
One of the three cranial fossa, the posterior fossa is a small hollow in the back of the skull. It contains the brainstem and cerebellum. Certain conditions can cause this area to become compressed. For example, if a tumor is located near the back of the skull, it will compress the cistern and reshape the brain.

The most effective way to diagnose a posterior fossa brain tumor is through MRI. The procedure is a series of basic MRI sequences that can be used to assess the structure of the brain. This protocol allows doctors to visualize lesions of the cranial nerves and the cerebellum. It can also be used to assess the cerebellum, the cranial nerve, and the CSF space.
Posterior Fossa Tumors Can Be Detected in Children Through MRI
In the past decade, a number of tumors of the posterior fossa have been detected in children through MRI. The corresponding posterior fossa MRI scans can be used to predict the risk of neurocognitive impairment in the patient. An MRI may help doctors determine the best treatment for a particular patient. During this procedure, a surgeon may reposition the brain or remove a portion of it.
Other research has focused on the clinical manifestations of these tumors. In adults, a tumor may be seen as a secondary symptom. If the symptoms of a primary posterior fossa brain tumor are present, the tumor can cause permanent damage to the area of the brain. MRIs will identify these tumours in patients and can be used to detect them in the brain. This type of diagnosis is important for treating childhood ependymomas.
Acute and chronic episodes of posterior fossa syndrome may be accompanied by cranial nerve palsies. The sixth cranial nerve controls eye movement. Damage to this nerve may lead to double vision and crossed eyes. The seventh cranial nerve is a facial nerve. If it is damaged, the child may not be able to make facial expressions and have difficulty moving his/her head.
Damage to the Nerves Can Cause a Drooping Face
Many people experience posterior fossa syndrome at some point in their lives. This syndrome is associated with cranial nerve palsies. In some cases, the affected cranial nerves control the eye movements. Children with this condition may have double vision or crossed eyes. Similarly, the seventh cranial nerve controls facial expressions. Damage to the nerves may result in drooping or drooping of the face.
In a recent study, two surgeons evaluated the effects of the tumor on the patient’s neurocognitive abilities and compared the results with their findings. The tumors were not associated with any neurological deficits. This study was published in the Asian PacJ Cancer Prev, where Yamauchi M. and Yamamoto A. conducted a retrospective review of posterior fossa brain tumors and the tumors in the posterior fossa.

The authors of the study note that patients with tumors in the posterior fossa are at a high risk for developing cognitive or emotional problems. They can potentially cause an individual to experience a variety of symptoms, including a loss of consciousness. In this situation, a continuous-flow shunt is a common treatment for hydrocephalus. However, this procedure is not recommended for all cases.
Reference:


